UCLA Study finds irritable bowel syndrome is not psychological
Finding removes the idea once and for all that IBS symptoms are not real and are “only psychological”
A large academic study has demonstrated structural changes in specific brain regions in female patients with irritable bowel syndrome (IBS), a condition that causes pain and discomfort in the abdomen, along with diarrhea, constipation or both.
A collaborative effort between UCLA and Canada’s McGill University, the study appears in the July issue of the journal Gastroenterology.
The findings show that IBS is associated with both decreases and increases in grey matter density in key areas of the brain involved in attention, emotion regulation, pain inhibition and the processing of visceral information.
IBS affects approximately 15 percent of the U.S. population, primarily women. Currently, the condition is considered by the medical field to be a “functional” syndrome of the digestive tract not working properly rather than an “organic” disorder with structural organ changes. Efforts to identify structural or biochemical alterations in the gut have largely been unsuccessful. Even though the pathophysiology is not completely understood, it is generally agreed that IBS represents an alteration in brain-gut interactions.
These study findings, however, show actual structural changes to the brain, which places IBS in the category of other pain disorders, such as lower back pain, temporomandibular joint disorder, migraines and hip pain — conditions in which some of the same anatomical brain changes have been observed, as well as other changes. A recent, smaller study suggested structural brain changes in IBS, but a larger definitive study hadn’t been completed until now.
“Discovering structural changes in the brain, whether they are primary or secondary to the gastrointestinal symptoms, demonstrates an ‘organic’ component to IBS and supports the concept of a brain-gut disorder,” said study author Dr. Emeran Mayer, professor of medicine, physiology and psychiatry at the David Geffen School of Medicine at UCLA. “Also, the finding removes the idea once and for all that IBS symptoms are not real and are ‘only psychological.’ The findings will give us more insight into better understanding IBS.”
Researchers employed imaging techniques to examine and analyze brain anatomical differences between 55 female IBS patients and 48 female control subjects. Patients had moderate IBS severity, with disease duration from one to 34 years (average 11 years). The average age of the participants was 31.
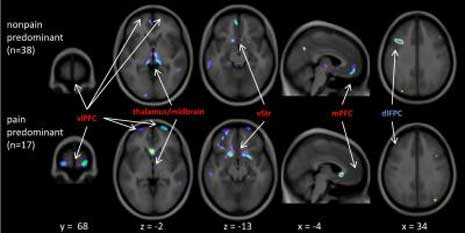
Investigators found both increases and decreases of brain grey matter in specific cortical brain regions.
Even after accounting for additional factors such as anxiety and depression, researchers still discovered differences between IBS patients and control subjects in areas of the brain involved in cognitive and evaluative functions, including the prefrontal and posterior parietal cortices, and in the posterior insula, which represents the primary viscerosensory cortex receiving sensory information from the gastrointestinal tract.
“The grey-matter changes in the posterior insula are particularly interesting since they may play a role in central pain amplification for IBS patients,” said study author David A. Seminowicz, Ph.D., of the Alan Edwards Centre for Research on Pain at McGill University. “This particular finding may point to a specific brain difference or abnormality that plays a role in heightening pain signals that reach the brain from the gut.”
Decreases in grey matter in IBS patients occurred in several regions involved in attentional brain processes, which decide what the body should pay attention to. The thalamus and midbrain also showed reductions, including a region — the periaqueductal grey — that plays a major role in suppressing pain.
“Reductions of grey matter in these key areas may demonstrate an inability of the brain to effectively inhibit pain responses,” Seminowicz said.
The observed decreases in brain grey matter were consistent across IBS patient sub-groups, such as those experiencing more diarrhea-like symptoms than constipation.
“We noticed that the structural brain changes varied between patients who characterized their symptoms primarily as pain, rather than non-painful discomfort,” said Mayer, director of the UCLA Center for Neurobiology of Stress. “In contrast, the length of time a patient has had IBS was not related to these structural brain changes.”
Mayer added that the next steps in the research will include exploring whether genes can be identified that are related to these structural brain changes. In addition, there is a need to increase the study sample size to address male-female differences and to determine if these brain changes are a cause or consequence of having IBS.
Literature:
University of California, Study finds structural brain alterations in patients with irritable bowel syndrome, Los Angeles, July 22, 2010.
Photo: UCLA
More interesting EMM Articles:
- CFS finally recognized as medical impairment under guidelines
- The psychogenic thesis for environmental diseases no value for science, destructive for legal rights
- MCS – Multiple Chemical Sensitivity a disease caused by toxic chemical exposure
- The department of Health of the Austrian Government recognizes MCS – Multiple Chemicval Sensitivity as a physical disease
- The naked truth about MCS – Multiple Chemical Sensitivity including foreword about German Situation

 A study of 145 preschool children reports, for the first time, that when the concentrations of two common phthalates in mothers’ prenatal urine are elevated their sons are less likely to play with male-typical toys and games, such as trucks and play fighting.
A study of 145 preschool children reports, for the first time, that when the concentrations of two common phthalates in mothers’ prenatal urine are elevated their sons are less likely to play with male-typical toys and games, such as trucks and play fighting.